
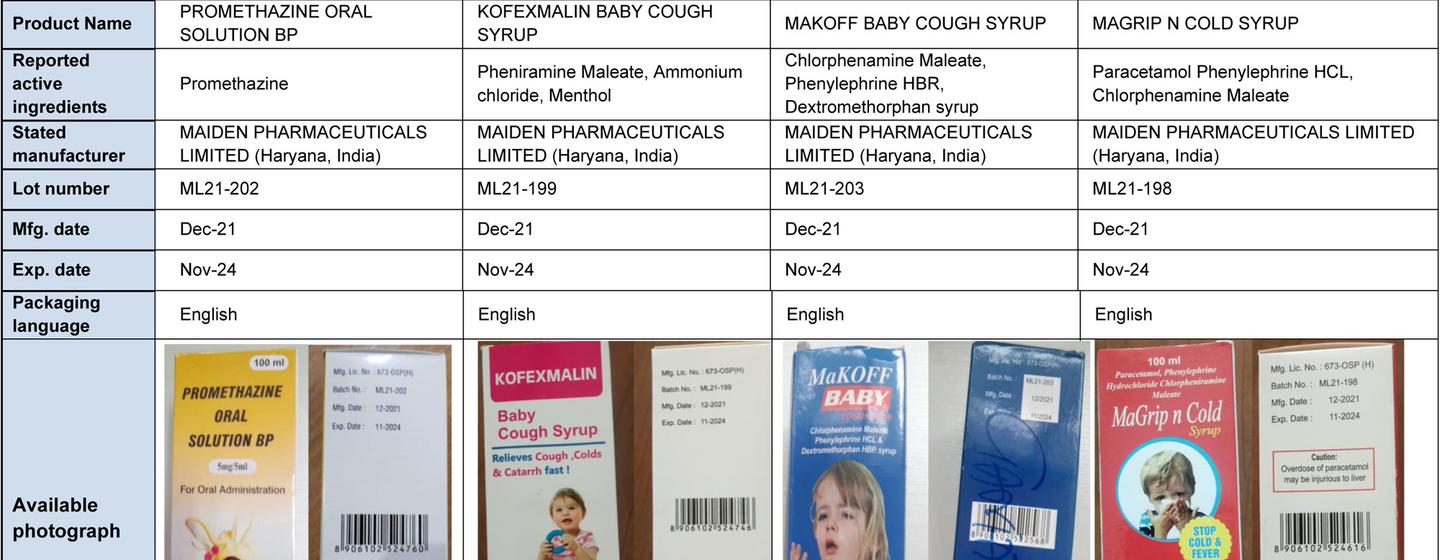
In the summer of 2022, 70 Gambian babies and young children died from kidney failure after ingesting cough syrup spooned out by their caregivers. The World Health Organization (WHO) issued a global alert that four tainted paediatric products had originated in India, as local health authorities continue to investigate how this tragedy unfolded.
This feature, which focuses on the illegal trade in substandard and fake medicines, is part of a UN News series exploring the fight against trafficking in the Sahel.
From ineffective hand sanitizer to fake antimalarial pills, an illicit trade that grew during the COVID-19 pandemic in 2020 is being meticulously dismantled by the UN and partner countries in Africa’s Sahel region.
Substandard or fake medicines, like contraband baby cough syrup, are killing almost half a million sub-Saharan Africans every year, according to a threat assessment report from the UN Office on Drugs and Crime (UNODC).
The report explains how nations in the Sahel, a 6,000-kilometre-wide swath stretching from the Red Sea to the Atlantic, which is home to 300 million people, are joining forces to stop fake medicines at their borders and hold the perpetrators accountable.
This fight is taking place as Sahelians face unprecedented strife: more than 2.9 million people have been displaced by conflict and violence, with armed groups launching attacks that have already shuttered 11,000 schools and 7,000 health centres.
Deadly supply meets desperate demand
Health care is scarce in the region, which has among the world’s highest incidence of malaria and where infectious diseases are one of the leading causes of death.
“This disparity between the supply of and demand for medical care is at least partly filled by medicines supplied from the illegal market to treat self-diagnosed diseases or symptoms,” the report says, explaining that street markets and unauthorized sellers, especially in rural or conflict-affected areas, are sometimes the only sources of medicines and pharmaceutical products.
Fake treatments with fatal results
The study shows that the cost of the illegal medicine trade is high, in terms of health care and human lives.
Fake or substandard antimalarial medicines kill as many as 267,000 sub-Saharan Africans every year. Nearly 170,000 sub-Saharan African children die every year from unauthorized antibiotics used to treat severe pneumonia.
Caring for people who have used falsified or substandard medical products for malaria treatment in sub-Saharan Africa costs up to $44.7 million every year, according to World Health Organization (WHO) estimates.

Motley trafficking
Corruption is one of the main reasons that the trade is allowed to flourish.
About 40 per cent of substandard and falsified medical products reported in Sahelian countries between 2013 and 2021 land in the regulated supply chain, the report showed. Products diverted from the legal supply chain typically come from such exporting nations as Belgium, China, France, and India. Some end up on pharmacy shelves.
The perpetrators are employees of pharmaceutical companies, public officials, law enforcement officers, health agency workers and street vendors, all motivated by potential financial gain, the report found.
Traffickers are finding ever more sophisticated routes, from working with pharmacists to taking their crimes online, according to a UNODC research brief on the issue.
While terrorist groups and non-State armed groups are commonly associated with trafficking in medical products in the Sahel, this mainly revolves around consuming medicines or levying “taxes” on shipments in areas under their control.
Snip supply, meet demand
Efforts are under way to adopt a regional approach to the problem, involving every nation in the region. For example, all Sahel countries except Mauritania have ratified a treaty to establish an African medicines agency, and the African Medicines Regulatory Harmonization initiative, launched by the African Union in 2009, aims at improving access to safe, affordable medicine.
All the Sahel countries have legal provisions in place relating to trafficking in medical products, but some laws are outdated, UNODC findings showed. The agency recommended, among other things, revised legislation alongside enhanced coordination among stakeholders.

States taking action
Law enforcement and judicial efforts that safeguard the legal supply chain should be a priority, said UNODC, pointing to the seizure of some 605 tonnes of fake medicines between 2017 to 2021 by authorities in the region.
Operation Pangea, for example, coordinated by UN partner INTERPOL in 90 countries, targeted online sales of pharmaceutical products. Results saw seizures of unauthorized antivirals rise by 18 per cent and unauthorized chloroquine, to treat malaria, by 100 per cent.
“Transnational organized crime groups take advantage of gaps in national regulation and oversight to peddle substandard and falsified medical products,” UNODC Executive Director Ghada Waly said. “We need to help countries increase cooperation to close gaps, build law enforcement and criminal justice capacity, and drive public awareness to keep people safe.”
UN in action
- WHO launched the Global Surveillance and Monitoring System, works with a Member State Mechanism on substandard and falsified medical products, monitors products, and issues alerts to its 194 members.
- The UN International Telecommunication Union (ITU) and WHO partnered on a focus group on the use of artificial intelligence for health.
- The UN Interregional Crime and Justice Research Institute (UNICRI) studies counterfeit products and their impact on consumer health and safety.
- The UNODC Strategic Vision for Africa 2030 includes more protection from falsified medical products, and its Good Legislative Practices on Combating Falsified Medical Product-Related Crime supports countries in enacting legislation and protecting public health.
- The World Customs Organization (WCO) and UNODC launched a container control programme in 70 nations to assist authorities in intelligence sharing and supply chain security.